Arrhythmias
Acute management of arrhythmias
- 12-lead EKG if possible and have defib pads on pt
- Is the pt unstable (hypotensive, signs/symptoms of hypoperfusion)?
- Is the information real?
- Review tele strips if stable: VUMC Web Resources -> VUH PIICiX Philips Web -> pt selection -> alarm review (vuhphilipsweb.app.vumc.org)
- Review past EKGs to determine if pt has had this rhythm before
- Ensure pt has good IV access
- Labs: BMP, Mg, TSH, and +/- troponin, tox screen
Bradyarrhythmia
Benjamin French
Background
- Sinus node dysfunction (pacing defect) vs atrioventricular block (conduction defect)
- Clinical presentation:
- A sinus HR > 50 bpm or a sinus pause < 3 seconds is unlikely to cause symptoms
- Symptoms include syncope/presyncope, dyspnea, angina
Potential etiologies
- Older age (most common)
- Ischemia (can’t miss)
- Metabolic: Hypothyroidism, hyper/hypokalemia, hypermagnesemia (generally > 8 mg/dL)
- Infection: Perivalvular abscess, Lyme, Toxoplasmosis
- Inflammatory/infiltrative: Myocarditis, SLE, cardiac sarcoidosis, amyloidosis, hemochromatosis
- Cardiac surgery/valvular procedures
- High vagal tone (e.g., pain, nausea, athletes)
- Sleep apnea (should be considered in nocturnal sinus bradycardia) Medications: Beta blockers, verapamil, diltiazem, digoxin, antiarrhythmics, alpha-2 agonists, antiepileptics, propofol, cannabis, etc.
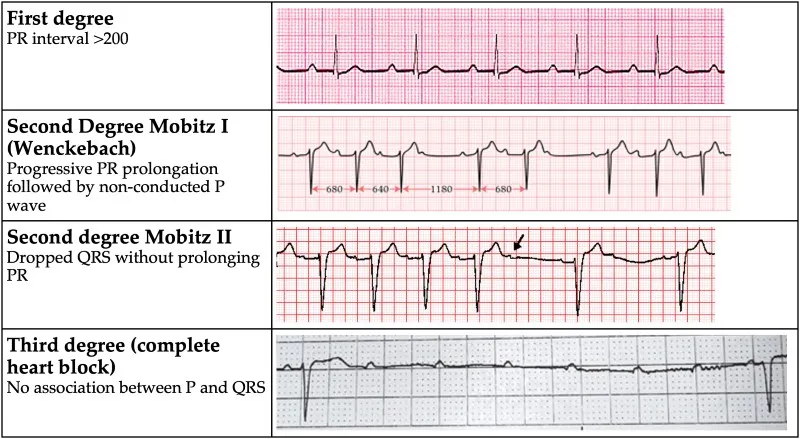
AV Block
Management
- Avoid nodal blocking agents – Adenosine, Beta-blockers, CCBs, Digoxin
- Observation if asymptomatic
- Treat identified underlying causes
- If symptomatic or high-grade block (Mobitz II or complete heart block), EP consult for pacemaker evaluation
- If unstable:
- Call CCU Fellow
↓
IV atropine (1 mg every 3 to 5 minutes; maximum total dose: 3 mg) Do NOT use in heart transplant
↓
Dopamine (5 to 20 mcg/kg/minute) OR Epi (2 to 10 mcg/min)
↓
Transvenous pacing
- Call CCU Fellow
Tachyarrhythmias - Narrow Complex
Cesar Campos
Background
- Three causes of tachyarrhythmias
- Re-entry: pt with structural heart disease (e.g. post-infarction scar)
- Abnormal Automaticity: electrolyte derangement or acute ischemia (Purkinje fibers)
- Triggered Activity: early and late after depolarizations. (e.g. Hypokalemia, ischemia, infracts, excess calcium and drug toxicity)
Evaluation
- Unstable tachyarrhythmia
- Start with treatment, determine type later
- Synchronized cardioversion: place defibrillator pads, consider 0.5-2mg IV midazolam for sedation, prepare for synchronized cardioversion at 200J (can ↑ to 300-360 J)
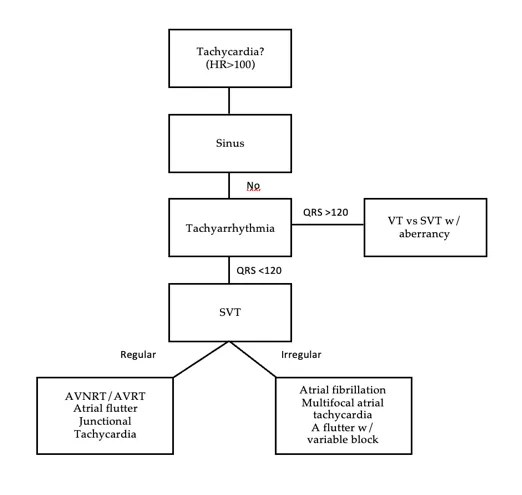
Tachyarrhythmia differential
Sinus tachycardia
- Maximum rate usually (220 - patient age)
- Management: Address underlying causes (eg, fever/sepsis, hypo/hypervolemia, anxiety, anemia, PE, ACS, hypoxia, pain, urinary retention, withdrawal)
Atrial Fibrillation/Flutter – See Atrial fibrillation section
Multifocal atrial tachycardia
- Mechanism/etiologies: multiple atrial premature beats from hypoxia/increased atrial pressure.
- Characteristics: ≥3 p wave morphologies. Irregular rhythm. Gradual onset and termination. Rate 100-150.
- Management: BBs and non-DHP CCBs can be effective, address underlying issue
- AVNRT/AVRT
Mechanism/etiologies:
- AVNRT - reentrant loop that involves the AV node and the atrial tissue causing simultaneous depolarization of the atrium and the ventricle.
- AVRT - Involves an accessory pathway that bypasses the normal insulation provided by the atrioventricular valves, allowing conduction between the atria and ventricles
Characteristics
- AVNRT: P wave rarely seen (buried in QRS).
- AVRT: in narrow complex (orthodromic), P after QRS; in wide complex (antidromic), P rarely observed (buried in T wave)
Management
- Vagal maneuvers (1st line): Sit pt upright -> have them blow into tip of 10cc syringe for 10-15 seconds -> rapidly lay supine and raise legs
- Adenosine (2nd line): therapeutic (break AVRT/AVNRT and 80% of atrial tachycardias) and diagnostic (allows visualization of underlying rhythm)
- Would try and have continuous 12 lead EKG on while pushing adenosine to try and catch the underlying rhythm
- Do NOT give in heart transplant, severe COPD, pre-excitation causing wide complex tachycardia (WPW → antidromic AVRT)
- Peripheral at AC or above w/ arm elevated: 6mg x1 → 6mg x1 (if not effective after 1-2 min) →12mg x1 (if refractory to 6mg)
- Central: cut dose in half to 3mg x1 → 3mg x1 → 6mg
Dosing
Drug |
Dosing |
Benefits |
Side Effects |
|---|---|---|---|
| Metoprolol |
5mg IV q5m x3 PO metop tartrate 12.5mg q6h, ↑ every 6h to target |
Good 1st line agent Less BP effect than dilt |
Hypotension, Negative inotropy |
| Diltiazem |
10-20mg IV over 2m q15m x2 drip = 5-15mg/h |
Good 1st line w/ normal EF with drip needed |
Hypotension Do NOT use in HFrEF |
| Esmolol |
500mcg/kg bolus drip = 50-200mcg/kg/min |
Rapid onset/offset RBC metabolism |
Hypotension |
| Amiodarone | 150 IV over 10-30m, then 1 mg/m for 6h, then 0.5mg/m for 18h |
Minimal BP effects Long lasting; Relatively fast onset (acute effect is mostly beta blockade) |
Pulmonary and thyroid toxicity Cardioversion |
| Digoxin | 500mcg IV x1, then 250mcg IV q6h x2-3 | Great for reduced EF, positive inotropy |
Slow onset Depends on vagal tone – poor in hyper- adrenergic states |
| Procainamide | 20-50 mg/min loading, 1-4 mg/min maintenance | Use in pre-excitation syndromes (i.e. WPW), does not inhibit AV nodal conduction |
Lupus-like syndrome Hypotension |
Tachyarrhythmias - Wide Complex and PVCs
Cesar Campos
Definitions
- Premature Ventricular Complex (PVC): early ventricular depol +/- mechanical contraction
- PVCs are common: Up to 80% of apparently healthy people have PVCs
- PVC induced cardiomyopathy may be present with PVC burden >10-20%
- Inpt Eval: Order 12 lead EKG to look for conduction disease (Long QT, brugada), K, Mg, TSH, Drug screen (EtOH, nicotine, stimulants, caffeine), med rec for QT prolonging agents, tele to assess PVC burden
- Inpt management: consult to EP for PVCs rarely warranted unless significant PVC burden (>5 PVC/min, consistently) in setting of reduced LVEF.
- For pts with >5 PVC/min or pts with symptoms, discharge with Ziopatch (VA) or mobile cardiac telemetry (VU) and obtain TTE if not done in past 3 months.
Ventricular tachycardia: a run of 3+ PVCs
- Sustained VT: VT for >30 seconds or shorter if it requires intervention
- Nonsustained VT (NSVT): VT for < 30 seconds
- VT storm: 3+ separate episodes of sustained VT within 24 hrs.
VT Morphologies
- Monomorphic VT: similar QRS configuration from beat to beat
- Usually 2/2 scar-mediated VT from prior infarction
- Polymorphic VT: a continuously changing QRS configuration from beat to beat
- Ischemia until proven otherwise
- Torsades de Pointes: a form of polymorphic VT with a continually varying QRS that appears to spiral around the baseline of the ECG in a sinusoidal pattern
- Ventricular fibrillation (VF): chaotic rhythm characterized by undulations that are irregular in timing and morphology, without discrete QRS complexes
- Wide-complex tachycardia (WCT): QRS >0.12 seconds and HR >100 beats/min
Wide-complex tachycardia evaluation
- WC-caused by ventricular arrhythmias (ventricular tachycardia or ventricular fibrillation) or supraventricular tachycardias with aberrant conduction resulting from one of the following: disease in the His–Purkinje system, such as left or right bundlebranch block; a bypass tract (i.e., Wolff–Parkinson–White syndrome), with depolarization of the ventricle from the bypass tract; or a ventricular paced rhythm from a pacemaker.
- Of note, a bundle branch block may appear with faster or slower heart rates and disappear with normal heart rates (ie, rate dependent).
- To differentiate between WCTs:
- Regular WCT: monomorphic VT or SVT with aberrant conduction
- Look at baseline rhythm: If QRS morphology identical to those seen in sinus rhythm, likely SVT with aberrant conduction; if not, likely monomorphic VT
- If AV dissociation present and ventricular rate faster than, atrial rate, then it is likely VT.
- If an escape beat or fusion beat is seen, this would also support VT
- If AV dissociation present and ventricular rate faster than atrial rate, likely VT
- Positively or negatively concordant QRS complexes in precordial leads suggest VT.
- Irregular WCT: atrial fibrillation with aberrant conduction (if same QRS morphologies) or polymorphic VT (if different QRS morphologies)
- Regular WCT: monomorphic VT or SVT with aberrant conduction
Management
Unstable
- Sedate with midazolam 1-2mg
- Cardioversion for monomorphic VT. Synchronized shock at 100-200J
- Defibrillation if VF/polymorphic VT
Stable
Drug Name |
Dosing |
Side Effects |
|---|---|---|
| Amiodarone (class III) | 150mg IV over 10 min, then 1mg/min for 6 hours; repeat bolus if VT recurs | Bradycardia, hypotension (acutely) |
| Lidocaine (class IIB) | 1-1.5mg/kg (usually 75-100mg) at a rate of 25-50mg/min; lower doses of .5-.75mg/kg can be repeated every 5-10min as needed | Slurred speech, AMS, seizures, bradycardia |
| Procainamide (class IA) | 20-50mg/min until arrhythmia terminates or max dose 17mg/kg is reached |
Bradycardia, hypotension, torsades, drug-induced lupus Avoid in HF pts, prolonged QT |
- Cardioversion if refractory to medical management
- Treatment of underlying cause if identifiable: Ischemia, electrolyte disturbances, heart failure, drugs
