Right Heart Catheterization
Ahmad Yanis
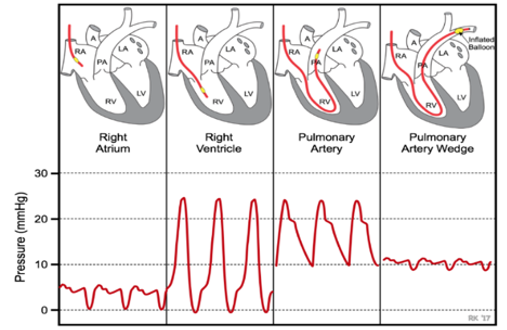
Pulmonary artery catheter (PAC): Multi-lumen catheter that sits in the right heart to provide invasive measurement of hemodynamic parameters
Indications for PAC Placement
Diagnose undifferentiated shock, Severe cardiogenic shock, Diagnose pulmonary hypertension, Diagnose left -> right shunting, Diagnose valvular and pericardial disease, Titrating medications (specifically inotropes, pulmonary vasodilators, diuresis)
Contraindications to PAC placement
- Infection at the insertion site
- RA/RV mass or thrombi
- Proximal pulmonary artery embolism
- Tricuspid or pulmonic valve endocarditis
- Mechanical tricuspid or pulmonic valves
- Presence of RV assist device
Complications of PAC placement
- Arrythmias: VT, RBBB, 3rd degree AV block if preexisting LBBB
- Infection (endocarditis of the pulmonary valve)
- Bleeding
- Pulmonary embolism and pulmonary Infarct
- Pneumothorax
- Air embolism
- Pulmonary artery perforation / rupture
- Endocardial/valvular damage
Definition |
Normal 'Rule of 5s' |
Interpretation |
|
|---|---|---|---|
| Central Venous Pressure(CVP) | Pressure in superior vena cava, often an indicator of volume status | 0 - 5 mmHg |
Elevated CVP: cardiac dysfunction and/or hypervolemia Low CVP: volume depletion or decreased venous tone |
| Right Atrial Pressure (RAP) | Surrogate for preload, should be same as CVP | 0 - 5 mmHg | Elevated RAP: disruption in forward cardiac flow or hypervolemia |
| Right Ventricle Pressure | Right ventricular systolic* and end diastolic pressures | 25/5 mmHg | Elevated RVP**: -PA/PV disorder: pulm HTN, PV stenosis, PE -RV disorder: CM, tamponade, ischemia/ infarction |
| Pulmonary Artery Pressure (PAP) | Measured as systolic, diastolic, and mean pressures. Diagnoses pHTN. |
25/10 mmHg Mean: 15 mmHg |
Elevated PAP: -Acute: PE, hypoxemia induced pulmonary vasoconstriction -Chronic: PH groups 1-5 |
| Pulmonary Artery Wedge Pressure (PAWP or wedge) | Surrogate for left atrial pressures and LVEDP | 10 mmHg | Elevated PAWP (LVEDP): LVHF, mitral and aortic valve disorders, hypervolemia, R to L shunts, constrictive/ restrictive CM, HOCM |
| Thermodilution Cardiac Output & Index | Amount of blood pumped in one min. CI is the cardiac output divided by body surface area (to standardize for body size) |
CO: 3.4-15 L/min CI: 2.8-4.2 L/min/m^2 |
Low CI: systolic/diastolic heart failure, severe valvular disorder (MR, AS), RV failure, pHTN, cardiogenic shock. Elevated CI (high-output state): sepsis, anemia, thyrotoxicosis, A-V shunt |
| Mixed central venous oxyhemoglobin saturation (SvO2) | % of oxygen bound to Hgb in blood returning to the right side of the heart, reflects total body O2 extraction | 65-70% |
High SvO2 (> 65%): -Decreased O2 demand -High flow states seen in distributive shock (sepsis) Low SvO2 (< 50%): decreased O2 delivery seen in cardiogenic or hypovolemic shock |
|
* RVSP can be a surrogate for PASP **Severe RVP elevations are generally chronic while acute conditions typically have RVSP <40-50 |
|||
Calculating Hemodynamic Parameters from PAC Pressures
|
|
Definition |
Normal Values |
Interpretation |
|---|---|---|---|
| Fick CO and CI | Calculated CO based on Oxygen consumption (VO2), Hbg, and O2 sats of arterial and venous blood |
4-7 L/min 2.5-4 L/min/m2 |
See "Cardiac Index" above. |
| Systemic Vascular Resistance (SVR) | Measurement of afterload; helpful in delineating the etiology of shock as well as guiding afterload-reduction therapy in HFrEF | 700-1200 dynes*s*cm-5 |
Elevated SVR: hypovolemic, cardiogenic, and obstructive shock Decreased SVR: distributive shock (sepsis, anaphylaxis, neurogenic) |
| Transpulmonary gradient (TPG) | Differentiates between pre- and post-capillary pulmonary hypertension. MPAP minus PCWP |
< 12 mmHg | A TPG value greater than 12 mmHg indicates that a component of the pHTN is secondary to pulmonary vascular disease |
| Pulmonary Vascular Resistance (PVR) |
Gold standard in the estimation of the severity of pre-capillary pHTN Reflects the pressure drop across the pulmonary system only and is independent of the LA, mitral valve and the LV TPG / CO |
< 3 Wood Units 30-90 dynes*sec*cm5 |
Elevated PVR (>3 Wood units) suggests pre-capillary pHTN Normal PVR seen in pulmonary venous hypertension (diastolic dysfunction) |
| Pulmonary artery pulsatility index (PAPi) | Pulmonary pulse pressure relative to preload (RAP), Indicator of RV function PA Pulse Pressure / CVP |
>3.0 = normal 2-3 = mild RV dysfx 1-2 = moderate RV dysfx <1 = severe RV dysfx | PAPi < 0.9 predicts in-hospital mortality and/or need for RVAD in acute MI. Can be decreased in pure RV failure or biventricular failure |
| Cardiac Power | Cardiac output relative to afterload, a measure of LV contractile reserve CPO = (Mean Arterial Pressure (MAP) x Cardiac Output (CO)) / 451 |
Normal > 1 |
CP< 0.6 strongly suggestive of LV failure Found to be a strong independent hemodynamic correlate in pts with cardiogenic shock. Predictor of mortality in CCU |
