Liver Transplant (LT) Workup
Katelyn Backhaus
Background
- Model for End-stage Liver Disease (MELD-Na) score: initially developed to predict survival following TIPS placement, though is now used to objectively rank patients in terms of priority for liver transplant (LT)
- Factors in total bilirubin, creatinine, INR, and Na.
- Exception points given for complications like HCC and hepatopulmonary syndrome (HPS), leading to score in mid to high 20’s even if biologic MELD is low
- Highest score lasts for 7 days
- Listing a pt for LT is determined by a multidisciplinary transplant committee
- Acute liver failure pts take precedence over decompensated cirrhosis pts for LT
Indications |
Contraindications* |
|---|---|
| Cirrhosis with MELD ≥ 15 or evidence of decompensation (ascites, variceal bleed, HE, HPS, portopulmonary HTN) | Ongoing substance abuse (must have documented abstinence ≥ 3 mos) – refer to exception policy in Alcoholic Hepatitis section |
| Acute liver failure | Untreated or recurrent malignancy or metastatic disease |
| HCC that meets Milan criteria | Active infection, AIDS (CD4 <200) |
| Pts with early hilar cholangiocarcinoma that meets specific criteria | Documented history of medical noncompliance |
| Other rare diseases (e.g., familial amyloid polyneuropathy or hyperoxaluria) | Lack of adequate social support |
| Anatomic contraindications: chronic cardiac/pulmonary conditions that significantly increase perioperative risk (e.g., severe pulm HTN) | |
| Fulminant hepatic failure with sustained ICP >50mmHg or CPP <40mmHg | |
| Class III Obesity (BMI>40) is a relative contraindication (class 2B) | |
| * Advanced age (>70) is not itself a contraindication but candidates >70 should be almost free of comorbidities to be considered | |
Evaluation
- Abdominal CT (triple phase) or MRI (multiphase with contrast) to evaluate for hepatic malignancy and vascular anatomy
- Infectious workup: TB testing, HIV, RPR, VZV, CMV, EBV, and Hepatitis A, B, and C
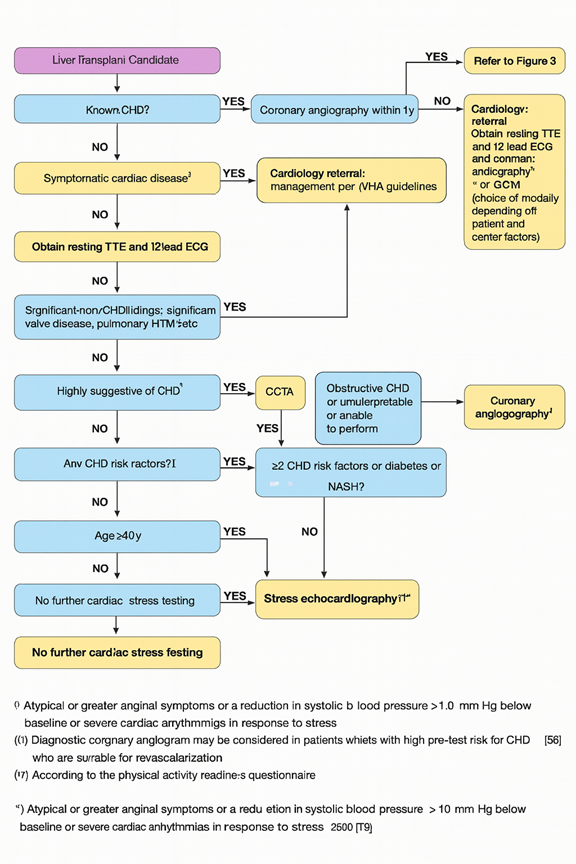
- Cardiac evaluation:
- If RVSP > 40mmHg on TTE, then R Heart Catheterization is indicated
- PFT’s, carotid US
- Panorex to identify dental disease; consult OMFS pending results
- Appropriate cancer screenings (CXR in all patients, CT Chest in prior/current smokers, colonoscopy, pap smear, mammogram, and PSA if applicable)
- DEXA scan (osteoporosis in up to 55% of individuals with cirrhosis)
- Certification of completion of intensive outpatient program (IOP) for substance abuse - Evaluation by hepatobiliary surgical team after obtaining cross sectional imaging
- Psychosocial evaluation (consult Psychiatry, social work)
- Current VUMC policy: pts should be abstinent from alcohol for no less than 3-6 months, although exceptions may be made for early liver transplant based on a very strict protocol. Discuss exception criteria with attending if suspect patient unlikely to survive hospitalization without transplant
Both living and deceased donor transplants are offered at VUMC. Donor evaluation, however, cannot be started before the potential recipient is deemed a candidate. Of note, should consider possible simultaneous liver-kidney transplantation for 1) CKD <30mL/min after > 90 days of eGFR<60 or 2) AKI dependent on dialysis >8 weeks or if extensive glomerulosclerosis present.
