Ascites and Hepatic Hydrothorax
Thomas Strobel
Ascites
Background
- Associated with a reduction in 5-year survival from 80% to 30%.
- Most often due to portal HTN. Less common causes include peritoneal or metastatic cancer, CHF, TB, nephrotic syndrome, Budd-Chiari, sinusoidal obstructive syndrome (S.O.S), or complications from procedures and pancreatitis
Grade |
Definition |
Treatment |
|---|---|---|
| Grade 1 Ascites | Only seen on imaging | 2g Na restriction |
| Grade 2 Ascites | Moderate, symmetric abdominal distension | 2g Na restriction, diuretics |
| Grade 3 Ascites | Marked, tense abdominal distension | LVP + Na restriction, diuretics (unless refractory) |
Evaluation
- Bedside ultrasound on admission to confirm presence of ascites
- Diagnostic paracentesis in all pts with ascites on admission mainly to rule out occult SBP
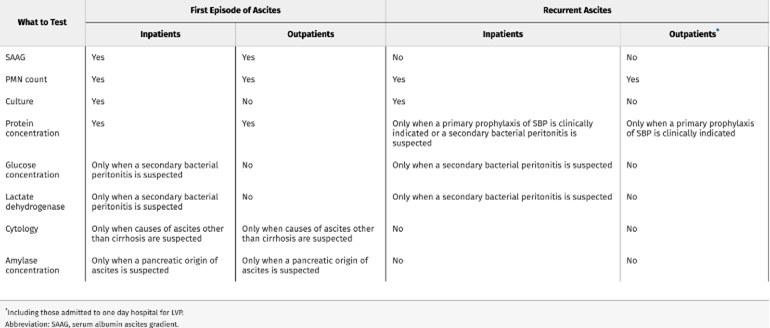
- Initial paracentesis or when cause of ascites is uncertain: ascitic fluid total protein, serum and BF Albumin, cell count w/diff, culture
- Subsequent/Serial paracenteses: cell count w/diff, culture, protein
- Always inoculate culture bottles at bedside
- Per AASLD guidelines elevated INR and thrombocytopenia (<50K) are not contraindications for paracentesis. Additionally, administration of clotting factors or platelets is not recommended. However, practically our procedure team often looks for INR < 3.5 (IR usually does not care about INR)
- Serum-ascites albumin gradient (SAAG) = serum albumin - ascites albumin.
Total Protein Ascites (not serum) |
SAAG ≥1.1 g/dL (Portal HTN) |
SAAG < 1.1 g/dL (Non-portal HTN) |
|---|---|---|
| < 2.5 g/dL | Cirrhosis | Nephrotic Syndrome Myxedema |
| ≥2.5 g/dL | Post-hepatic portal HTN: Cardiac Ascites Budd-Chiari |
Malignant Ascites Pancreatic Ascites TB |
- Other tests:
- Triglycerides: if fluid is milky
- Cytology: if very concerned for peritoneal carcinomatosis. May need up to 3 separate samples (50ml or more) to be able to detect malignant cells
- ADA: if concern for peritoneal TB
- Hematocrit: For bloody appearing fluid (not just serosanguinous) to rule out hemoperitoneum. There needs to be a recent serum HCT for comparison.
- Amylase: If concerned for pancreatic ascites
- Glucose, LDH if concern about secondary peritonitis (see below)
Refractory Ascites
Two distinctions
- Diuretic-resistant: lack of response to diuretics (max spironolactone 400mg/Lasix 160mg), Na restriction and rapid recurrence following paracentesis
- Diuretic-intractable: unable to tolerate diuretic therapy due to adverse drug effects (unexplained HE, AKI, K abnormalities, hypoNa, intractable muscle cramps)
Management aside from liver transplant
- Discontinue diuretics once refractory ascites has been established, but continue Na dietary restriction
- Consider oral midodrine; can be especially helpful if pt is also hypotensive
- Serial paracenteses, generally arranged OP with IR
- Consider TIPS (trans jugular intrahepatic portosystemic shunt; has survival benefit) for refractory ascites or recurrent ascites (>3 LVPs in one year despite compliance with diet and diuretics). Following TIPS, cessation or decrease in ascites should occur in ~6 weeks
- Consider discontinuing beta blockers in patients with refractory ascites if sBP <90, SCr >1.5, or Na <130
