Cardiac Devices
Daniela Gomez Zubieta
1. Pacemakers:
A device that maintains or restores a normal heart rhythm by stimulating the myocardium.
- Peripheral permanent pacemakers (PPMs)
- SubQ generator, transvenous leads
- Single chamber: RV (most common) or RA lead
- Dual chamber: RV and RA leads
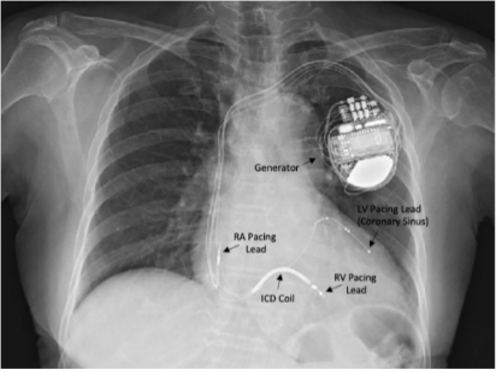
- BiV (CRT- cardiac resynchronization therapy): RV, RA, and LV (coronary sinus) leads
- SubQ generator, transvenous leads
- Leadless pacemaker (Micra)
- Implanted generator in RV; Indication: (class 1 indications below, refer to ACC/AHA guidelines for class 2 and 3)
- Sinus node dysfunction (sinoatrial exit block, sinus pause, sinus bradycardia, tachy-brady syndrome)
- AV block (Mobitz II ,3rd degree, 2nd degree of any kind w/ symptomatic bradycardia, chronic bifasicular block
- Persistent symptomatic 2nd or 3rd degree block after acute MI
- Neurocardiogenic syncope
- Implanted generator in RV; Indication: (class 1 indications below, refer to ACC/AHA guidelines for class 2 and 3)
2. Implantable Cardioverter/Defibrillators (ICDs):
- Transvenous: defibrillation coil +/- pacing lead
- Detect and treat VT/VF
- Anti-tachycardic pacing (ATP)- attempts to pace out of VT to prevent a shock
- Defibrillation if ATP unsuccessful
- Subcutaneous: defibrillation only, all extravascular
- Indications:
- Primary prevention
- HFrEF
- EF <35% and NYHA II-III or EF <30% and NYHA I
- Must be >90d from revasc, >40d from MI, and on GDMT >90d if nonischemic
- HFrEF
- Arrhythmogenic syndromes
- Arrhythmogenic RV cardiomyopathy, Brugada syndrome, HCM and cardiac sarcoid with specific risk factors
- Secondary prevention
- Sudden cardiac death
- Sustained VT/VF (spontaneous sustained, cardiac arrest 2/2 VT/VF)
- Inducible VT on EP study with history of syncope
- Primary prevention
3. Cardiac Resynchronization Therapy (CRT)
- BiV pacer that coordinates LV/RV contraction through synchronized activation of each ventricle following atrial contraction.
- P: CRT pacing only
- D: ICD function
4. LVADs:
augment cardiac output for end-stage heart failure
Examples of Common Pacing Modes on PPM:
- VVI: Single RV lead that delivers a beat if no beat sensed. Often used with chronic AF with bradycardia
- DDDR: Senses and paces both the atria and ventricle. If beat not sensed within a predefined interval, beat delivered. R indicates rate responsivity (changes rate based on changes in pt activity)
- Magnet: Paces at a fixed rate without respect to native electrical activity (AOO,VOO,DOO). Deactivates ICD shock. Often used in surgery or at end of life to avoid ICD shocks
Peri-Procedural Anticoagulation:
- - NOAC: hold 24-72h before procedure and 24-72h following procedure
- - Warfarin: continue through procedure
- - Antiplatelet: continue through procedure
- - Heparin and heparin related products to be avoided peri-implantation due to higher rates of pocket hematoma
Placement Complications
- Pocket hematoma
- Cardiac Tamponade
- Pneumothorax
- Infection
- Myocardial Perforation
- Lead Displacement
- Lead Disconnection
Long term Complications
- Secondary device Infection
- Lead fracture (lead lifetime 10-15 years)
- Insulation failure
The Pacemaker ID app is free and is useful for identifying device brand for interrogation When differentiating PPM vs. ICD, look for a coil and charge generator to identify the ICD.