Bedside Echocardiography
Matthew Gayoso
Finding an Ultrasound
- MICU: radiology room behind charge nurse's desk in middle hallway
- VA ICU: In front of resident workspace
- 8N: Behind nurses' station before entering cleaning supply room
- 8S: In supply closet to left as your walk toward nursing station - (door code is 1-3-5)
- 6MCE: COVID restricted (ask nurses)
- CCU/5N only: supply room on left as entering CCU
- Round wing: 5th floor, ask nurses
TTE Standard Views
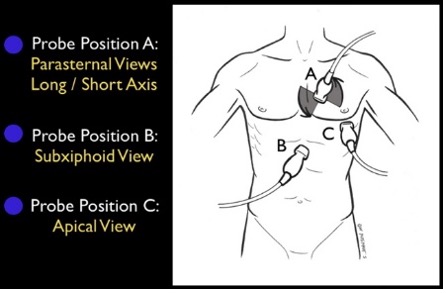
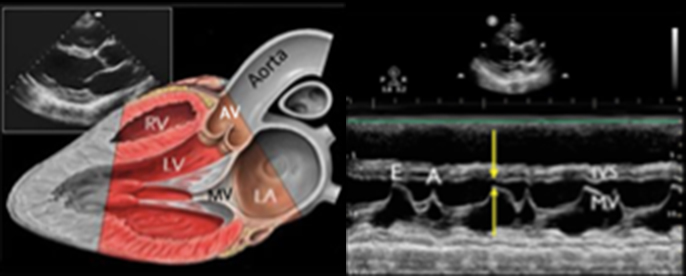
Parasternal Long
- Probe position: Rotate probe 180 degrees with right edge of probe/probe marker pointing toward pt’s left shoulder
- Make sure probe is centered over mitral valve (In right spot if you can see MV and AV)
E Point Septal Separation (EPSS)
- Distance separating the anterior MV leaflet from the septal wall as measure of LV systolic function (easy evaluation of systolic function)
- Place M mode spike at tip of mitral leaflet and hit M mode (perpendicular to septum)
- Identify E point (passive filling of LV) and determine distance from interventricular septum (IVS)
- Confounders that elevate EPSS: AR, MS
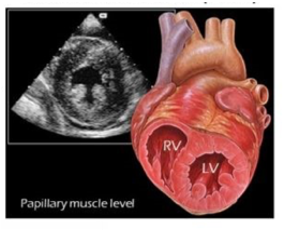
Parasternal Short
- Probe position: Rotate probe 180 degrees with right edge of probe/probe marker pointing toward pt’s left shoulder
- Good position to assess EF by visualizing wall thickening
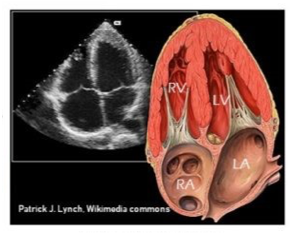
Apical Four Chamber
- Probe position: Slide down and look near pt’s left nipple (or in the intermammary fold after lifting up breast tissue if needed - at PMI if able to palpate
- Good to assess EF by visualizing cardiac shortening
Subxiphoid
- Probe position: Push probe head into pt’s abdomen just below xiphoid and flatten probe to make nearly parallel to pt’s position, marker to pt’s left
- Troubleshooting: shift probe slightly left of midline (toward pt’s right) and angle toward heart/right to use liver as acoustic window or ask pt to take big breath (moves heart closer to probe)
- Best window to visualize pericardial effusion
IVC
- Probe position: subxiphoid area with probe marker facing toward pt’s head tilted slightly left of midline, trace IVC into RA to verify correct vessel (vs aorta)
- IVC size and collapsibility used as a surrogate for CVP and RAP
- <2.1cm and >50% collapse: RAP ~3 mmHg
- <2.1cm and < 50% collapse or >2.1cm and >50% collapse: RAP ~8 mmHg
- >2.1cm, <50% collapse: RAP ~ >15 mmHg