Dementia
Normal Aging |
Mild Cognitive Impairment |
Alzheimer’s Dementia (DSM V Diagnostic Crit.) |
|---|---|---|
|
|
|
| Cognitive domains: learning/memory, language, executive function, complex attention, perceptual motor, social cognition | ||
Alzheimer’s Disease |
Vascular Dementia |
Lewy Body Dementia |
Frontotemporal Dementia |
|
|---|---|---|---|---|
| Onset | Gradual | Sudden or stepwise | Gradual | Gradual (age < 60) |
| Cognitive Domains & Symptoms | Memory, language, visuospatial | Depends on location of ischemia | Memory, visuospatial | Executive dysfunction, personality changes, disinhibition language, +/- memory |
| Motor Symptoms | Rare early; Apraxia later | Correlates with ischemia | Parkinsonism (memory loss typically precedes) | None |
| Progression | Gradual (over 8-10 years) | Gradual or stepwise with further ischemia | Gradual, but faster than Alzheimer’s disease | Gradual, but faster than Alzheimer’s disease |
| Imaging | Possible global atrophy | Cortical or subcortical on MRI | Possible global atrophy | Atrophy in frontal & temporal lobes |
Rare causes of dementia: Parkinson disease dementia, posterior cortical atrophy, CJD, corticobasal degeneration, neurosyphilis, NPH, autoimmune dementias (eg, NMDA)
Evaluation
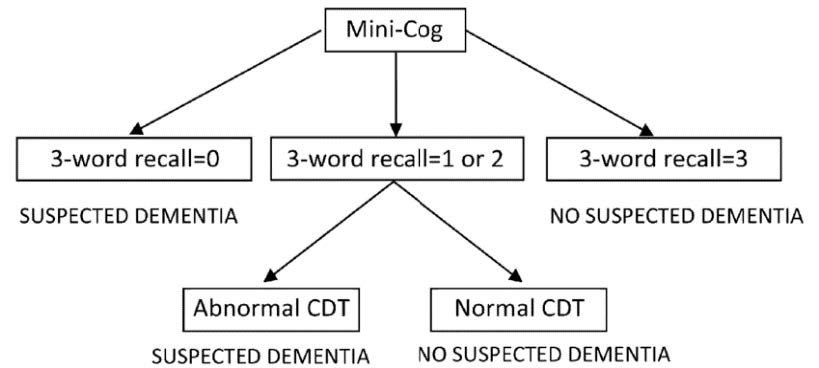
- MINI-COG: Screening test for cognitive impairment (highly sensitive)
- Word Recall: Ask pt to remember three words (banana, sunrise, chair). Ask pt to repeat immediately
- CDT: Ask pt to draw clock. After numbers are on the face, ask pt to “set hands to 10 past 11”
- Correct is all numbers in right position AND hands pointing to the 11 and the 2
- Ask pt to recall the three words
MOCA: Montreal Cognitive Assessment
- Lengthier test of cognition (but highly specific for cognitive impairment)
- Useful for detecting subtle deficits as in Mild Cognitive Impairment (MCI)
- Training and Certification is mandatory for proper use.
- Scores:
- 18-25: Mild cognitive impairment
- 10-17: Moderate cognitive impairment
- <10: Severe cognitive impairment
- Rule out reversible causes of dementia-like symptoms: DEMENTIA
- Drugs o Emotional (depression)
- Metabolic (CHF, COPD, CKD, OSA)
- Endocrine (hypothyroidism, hyperparathyroidism, hyponatremia)
- Nutrition (B12 deficiency)
- Trauma (chronic SDH)
- Infection (RPR, HIV testing in at-risk patient groups)
- Arterial (vascular- consider MRI brain)
- Consider referral for Neuropsychiatric testing if diagnostic pattern unclear. Consider MRI brain with contrast if concerned for inflammatory or infectious causes.
Management
- Targeting Cognitive Impairment
- Cholinesterase Inhibitors: Donepezil, rivastigmine
- Indicated for any stage of AD, PDD, LBD, Vascular Dementia (avoid in FTD)
- No role in dementia prevention
- SE: GI (nausea, diarrhea), bradycardia, orthostasis
- Cholinesterase Inhibitors: Donepezil, rivastigmine
- NMDA antagonists: Memantine
- Indicated in moderate to severe AD in combination with cholinesterase inhibitors
- Fewer SE than cholinesterase inhibitors
- Targeting Behaviors
- BPSD: Behavioral and psychological symptoms of dementia
- Non-pharmacologic management has the best evidence of effectiveness
- treat underlying cause, hydration/nutrition, orient, mobilize, manage pain, environmental modification, eliminate devices, engage family, sensory restoration, sleep protocol
- Depression: Treat with antidepressants (SSRI’s)- (citalopram 10mg or sertraline 25mg = starting doses
- Sleep Disturbance: Mirtazapine (7.5 mg nightly) or Trazodone (25 mg nightly)
- Agitation: SSRI (typically first line)- see above; mood stabilizers (manic-type behaviors)- Depakote 125mg q12 = starting dose (serum level 50-100 mcg/mL therapeutic)
- Consider antipsychotics (black box warning increased risk of death for older adults with dementia-related psychosis) for behaviors that threaten safety of patient or staff and use lowest dose possible
- See “Delirium” section in Psychiatry for inpatient management recommendations
