Chest Tubes
Jacob Lee
Background
Nomenclature |
Size |
Insertion Technique |
Specific Indications |
|---|---|---|---|
| Small Bore - Straight or Pigtail (coiled at the end to prevent dislodgement) | ≤14F | Seldinger | PTX, uncomplicated pleural effusions, initial empyema drainage (BTS guidelines) |
| Medium-Bore | 15-23F | Seldinger or Surgical | Larger pleural effusions or complex/exudative effusions |
| Large-Bore (Surgical) | 24-40F | Surgical Thoracostomy | Post-operative drainage, hemothorax, thick exudative effusions |
- Other Indications and Considerations
- Malignant effusions and hepatic hydrothorax are generally palliative measures only
- Large-bore/surgical chest tube should be placed for acute hemothorax, not pigtail
- Smaller size results in less tissue disruption but more likely to clog or kink
- Contraindications:
- Absolute: need for emergent thoracotomy
- Relative: Coagulopathy (INR Goal < 2-3 depending on proceduralist comfortability), large pulmonary bullae, pleural/pulmonary adhesions, skin infection at insertion site
Placement
- Consult pulmonology – they will decide whether interventional pulmonology/radiology needs to place the tube
- Location: related to pathology
- Pneumothorax - anterior near the apex of the lung in the 2nd intercostal space, midaxillary line
- Effusion (water, pus, blood, chyle) – depends on where the fluid is located but in general placed posterior near the base of the lung (fifth or sixth intercostal space, midaxillary line
- Potential complications: organ damage/perforation (lung, heart, diaphragm, intraabdominal), trauma of the intercostal neurovascular bundle, subcutaneous emphysema, pneumothorax, infection, re-expansion pulmonary edema.
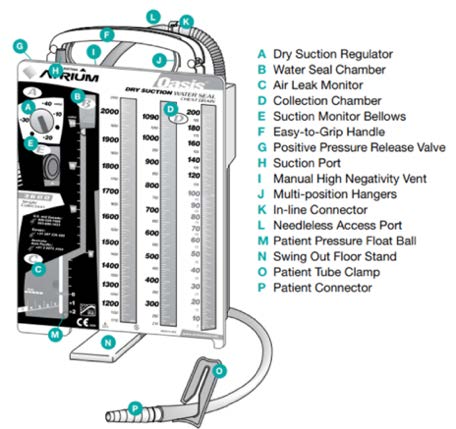
Understanding the Atrium
After the chest tube is placed, it is connected to the Atrium which can be connected to the wall for suction. (See Diagram below)
- (A) Dry suction control- determines the level of suction out of the chest tube and is set by the provider (typically -20 cm H2O). It is important to note that while the atrium is linked to the wall suction via suction port (H) the level of chest tube suction is determined by (A), regardless of what the wall suction setting is
- (B) Water seal chamber- if the atrium is disconnected from the wall suction, it is on “water seal” (i.e., to gravity). This allows for the one-way flow of pleural space contents out of the chest. This space also shows ‘tidaling’ in certain instances explained below
- (C) Air leak monitor- if air bubbles are present in the water seal chamber, then that indicates the presence of air in the pleural space.
- (D) Collection chamber- drains the pleural fluid contents via the chest tube.
- (E) Suction verification window- will be orange if suction is on and atrium is functioning appropriately
Normal Findings and Troubleshooting
- Tidaling: a normal finding referring to the rise (during inspiration) and fall (during expiration) of fluid in the water seal chamber
- Indicates communication between pleural space and the drainage system and that the system is functioning correctly
- Lack of tidaling can be seen in several instances: lung has fully re-expanded, chest tube is blocked (clogged/kinked), suction is turned on, or tube is dislodged/mispositioned
- Output in the absence of pathology can be up to roughly 150 cc/day which is the amount of fluid the pleural space produces daily
- In general, CXR is first study to order in evaluating a patient with a chest tube who undergoes a change in clinical status
- Air leaks: If bubbles are present in the water seal chamber, this indicates air in the pleural space. Intermittent bubbling is common in a PTX while air is still escaping from the pleural space. Continuous bubbling suggests an ongoing air leak. Two main categories of air leaks:
- Patient-related/originating from pleural space: Persistent air in the pleural space; seen in alveolar-pleural fistula, PTX (expected initially; should decrease over time as lung reexpands), mechanical ventilation
- System-Related/chest tube or drainage system: Air not originating from pleural space but the system; seen in chest tube dislodgement, faulty dressing seal at insertion site, cracked or damaged drain system.
- To identify the etiology of a new air leak, try clamping the chest tube
- Clamp near patient and bubbling stops → leak in pleural space
- Clamp near patient and bubbling continues → leak in the drainage system or tubing
- Clogging: Would see debris in the collection chamber and lack of tidaling in the water seal camber
- In pts with viscous fluid output (ex- empyema), important to flush the chest tube with normal saline flushes at least twice daily to prevent clogging
- For clog- try flushing 10cc of sterile saline toward the pt or “stripping” the chest tube by pressing the chest tube with your fingers and pulling towards the drainage system.
- always consult pulmonary for chest tube management unless another team (eg, thoracics) is actively managing
Removal
- Generally, chest tubes are removed when the underlying condition requiring their insertion has plateaued, improved, or resolved
- Effusions: less than 150 cc in 24 hours
- PTX: step wise approach. Usually once air leak resolves, will transition from wall suction to water seal with a CXR prior to transitioning and prior to removal. Generally guided by the team that placed the tube
- Chest tube should be removed while pt hums (to prevent inhalation during removal that could introduce air into pleural space). Pigtail catheters must be “unlocked” prior to removal to release the pigtail
