Lung Nodule
David Krasinski
Background
- Definition: focal, distinct radiographic density completely surrounded by lung tissue <3cm (mass >3cm – see “Lung Mass” chapter)
- Prevalence: 30% of all chest CTs. Most commonly are incidentalomas. >95% are benign. Larger and irregularly shaped nodules are more likely to be malignant.
Etiologies
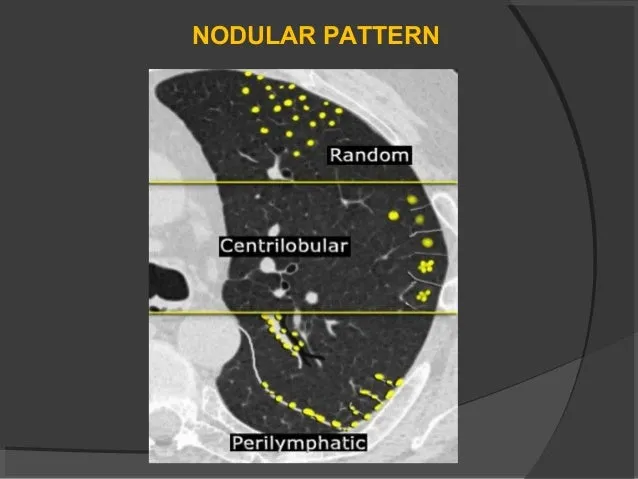
CT Pattern |
Pathology |
Etiologies |
|---|---|---|
| Random: hematogenous spread. | Infections | Miliary TB, septic emboli |
| Malignancy | Sarcomas, carcinomas | |
| Other | Langerhans cell histiocytosis | |
| Centrilobular: most diseases that track airways | Infectious | Granulomas from fungi, mycobacteria, prior bacterial infx (nocardia/S. aureus). |
| Inflammatory | Aspiration, hypersensitivity pneumonitis, bronchogenic cyst. | |
| Malignancy | Bronchogenic carcinomas (central: SCC, small-cell), peripheral (adenoCa, large cell) | |
| Peri lymphatic: lymph system spreadgret | Inflammatory | Sarcoidosis, pneumoconiosis |
| Malignant | Lymphangitic carcinomatosis, lymphoma, metastatic sarcomas/carcinomas | |
| Benign | Hamartomas, fibromas, hemangiomas, leiomyomas, amyloidoma. |
Management of solitary lung nodule
- History: hx of exposures (tobacco, asbestos, mining, biomass fuel), geographical epidemiology (histo/coccidio/TB), B-symptoms, personal and FxHx of malignancy
- Assess pt risk for malignancy
- High risk: >60yo, current smoker or heavy smoking history, history of cancer, FxHx lung cancer, irregular or spiculated, upper lobe, ≥2.3cm, double diameter or volume in past year
- There are online risk calculators (Brock, Mayo, Herder) helpful for providers who are not experts in lung nodule risk stratification
- Benign imaging features: central calcification, popcorn-like (hamartomas), laminated, stippled
- Consider Pulmonary referral if high risk features, known malignancy or recent history of malignancy, organ transplant or other immunocompromising condition, age <35yo
Fleischner guidelines for nodules <8mm
Risk for Malignancy |
Solid <6mm |
Solid 6-8mm |
Solid ≥8mm |
Subsolid (GGO ± solid component) |
|---|---|---|---|---|
| Low | No follow-up | CT at 6-12mo and consider at 18-24mo | Refer to Pulm. CT in 3mo. Consider PET + tissue sampling* | If >6mm, refer to Pulm. If malignant, may be slow growing. Requires follow up to 5 years. Initially every 6mo |
| High | Optional CT in 12mo | CT at 6-12mo and at 18- 24mo |
*Tissue sampling usually occurs via transthoracic needle biopsy (via IR), VATS (via thoracic surgery), or transbronchial biopsy (via interventional pulm).
ACCP 2013 Chest Guidelines for workup of nodules 8-30mm
Low to Moderate Risk Surical Risk
- Assess clinical probablility of cancer
- Very low (< 5%)
- CT surveillance
- Low/mod (5-65%)
- PET to assess nodule
- à Negative or mild uptate: CT surveillance OR nonsurgical biopsy
- àMod or intense uptake: nonsurgical biopsy or surgical resection
- High (> 65%)
- Standard stage eval (±PET)
- à No met: Surgical resection or SBRT or RFA
- à + Met (N2, 3): chemotherapy or chemoradiation (after biopsy)
- Very low (< 5%)
High Surgical Risk
- Nonsurgial biopsy OR
- Malignant
- Standard stage eval (±PET)
- à No met: Surgical resection or SBRT or RFA
- à + Met (N2, 3): chemother apy or chemoradi ation (after biopsy)
- Nondiagnostic
- CT surveillance
- Specific Benign
- Specific treatment
- Malignant
- CT surveillance
