Post-Procedural Care
Terra Swanson
Liver Biopsy
Percutaneous liver Bx (transabdominal approach)
- Patient have some abdominal pain that day and/or referred pain to the shoulder. Should improve by next day. Treat with pain medicine PRN. Avoid Toradol.
- Main risk is bleeding/hemoperitoneum. No routine follow up labs unless clinical concern for bleeding. If concerned, order stat H/H, call IR to discuss whether a triple phase CTA abdomen (noncontrast, arterial and venous phases) is warranted to look for active bleeding. o Wound care: will just have a bandaid, can come off in 24 hrs
Transjugular liver Bx (Neck, right internal jugular approach)
- Monitor right neck access for signs of hematoma. Transjugular biopsies have lower risk of bleeding but still possible, follow reccs as above if clinical concern. No routine labs.
- If gauze/Tegaderm present, this can be removed after 24 hrs and replaced with another bandage until skin nick heals.
- If dermabond present, leave intact and advise pt to not remove dermabond (it will fall off on its own).
TIPS (transjugular intrahepatic portosystemic shunt)
- Please ensure hepatology consult if not admitted to hepatology service after primary TIPS placement.
- Typically right IJ small incision access. Monitor for hematoma
- Patients often get a paracentesis intra-op if ascites is present, typically get albumin intra-op if >5L were drained
- Main post op concerns:
- Abdominal and/or neck pain to be expected post-TIPS. Monitor for increasing abdominal distention or neck hematoma.
- Hypotension can occur s/p TIPS. Consider albumin and IVF. If vitals not responding, obtain H/H and trend, touch base with IR to evaluate for risk of bleeding. If CT is warranted to eval for active bleeding: order a triple phase CTA abdomen/pelvis (noncontrast, arterial and venous phases).
- Monitor for signs of HE (hepatic encephalopathy) as more blood is being diverted away from liver and thus not being properly cleared of toxins. Pt may need to initiate lactulose if HE develops
- Monitor for signs heart failure after TIPS, usually they have a pre-op echo to assess for risk
- Routine post-op LFTS typically not necessary as LFTs expected to be elevated immediately after TIPS, unless there is another clinical indication to check them.
- Most patients can be discharged POD1 if no issues. Pt will have follow-up coordinated in IR at 1 month with a follow-up TIPS ultrasound around that time. Pt should also have follow-up with their hepatologist.
Post Renal Biopsy Monitoring and Complications (VUMC & VA)
Routine monitoring
- All pts are observed overnight in the hospital o Strict bed rest for 8 hrs following procedure followed by bed rest with bathroom privileges.
- Transplant bx: an abd binder with tennis ball is placed for 10 minutes post biopsy o (NOTE: this must be removed promptly to avoid compression injury/ATN)
- Frequent vital signs (q15 min x 4, q30 min x 4, q1h x 4, then q4h) You must inform the VA resident and preferentially the nurse at the VA who will be caring for your patient of these orders.
- Serial hct evaluation (at 0h, 4h, 8-12h, 18-24h) o Serial urine collection x 3(to assess for gross hematuria)
- Do NOT give SQ heparin (i.e., DVT prophylaxis), anti-platelet agents, or anticoagulating agents for 2 weeks post biopsy. If pt develops life threatening illness requiring anti-coagulation (e.g., ACS, DVT, PE) during this period, the renal fellow and attending should be notified immediately.
Clinical signs and symptoms of post-biopsy complication
- SBP <100, HR >120 or worsening hypertension from Page Kidney
- Gross hematuria
- Moderate or severe pain at biopsy site
- New onset of abd pain or loin pain o Evidence of bleeding (decrease in hct, increase in abd girth, abd/back ecchymosis)
Management of complications
- Bed rest
- Pain control
- Fluid resuscitation (for gross hematuria, “clot colic”)
- Maintenance of normal coagulation
- Imaging (renal ultrasound or CT scan of abd/pelvis) CT scan with contrast is better for visualizing extravasation. Discuss imagining type with your attending and maybe IR/Trauma.
- Transfusion of blood products
- Coil embolization by IR
- Surgical exploration or nephrectomy
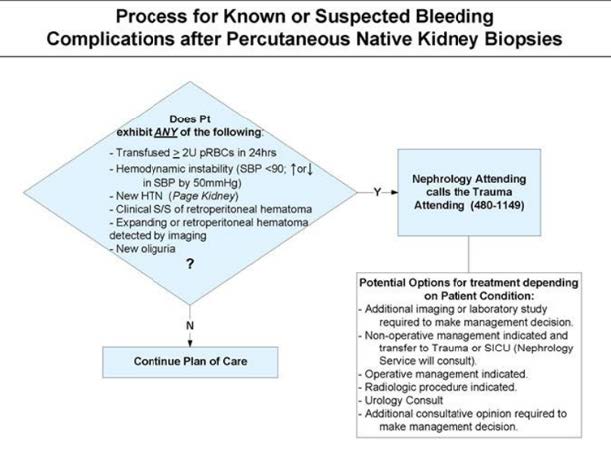
Protocol for management of post biopsy complications
- Renal fellow on call should be notified with a decrease in hct >3% pts, new or severe pain, significant hemodynamic changes (tachycardia or low or high blood pressure), or with any other significant post bx complication. The renal fellow or attending should help coordinate all consults and/or transfers.
- **Remember that if there is an acute bleed the hematocrit may be unchanged. In this setting tachycardia and blood pressure will be the first sign of a bleed.
- Ensure type and screen current; have cross matched blood available (if necessary); obtain serial hct checks and check frequent vital signs.
- If appropriate, transfer pt to unit with higher level of care. Pts with significant bleeding should be transferred to the Trauma ICU for management of penetrating renal trauma. Consultation of Interventional Radiology, Trauma Surgery, or Transplant surgery (for transplant biopsies) should be considered.
- Nephrology (or Transplant Nephrology) attending on call and attending who performed biopsy should be notified of any complications immediately!
