Stroke
Background
- Sudden onset, focal (usually unilateral) neurologic deficits: Weakness, sensory loss, vision loss, ataxia/unsteadiness, vertigo, double vision, facial droop, dysarthria, aphasia
- Differential
- Stroke (ischemic or hemorrhagic)
- Seizure or post-ictal paralysis
- Headache phenomena (complex migraine)
- Spinal cord lesions, though these more commonly cause bilateral symptoms
- Stroke-like symptoms can also develop as recrudescence–previous stroke or brain lesion symptoms worsening with systemic toxic, metabolic, infectious processes or hypotension
Evaluation
- Critical decision-making information: Last time pt was at their neurologic baseline (last known normal - LKN), time symptoms first observed, anticoagulation status, recent surgeries, history of bleeding (severe GIB or ICH), recent medications, blood pressure, blood sugar, platelet count, and baseline neuro exam
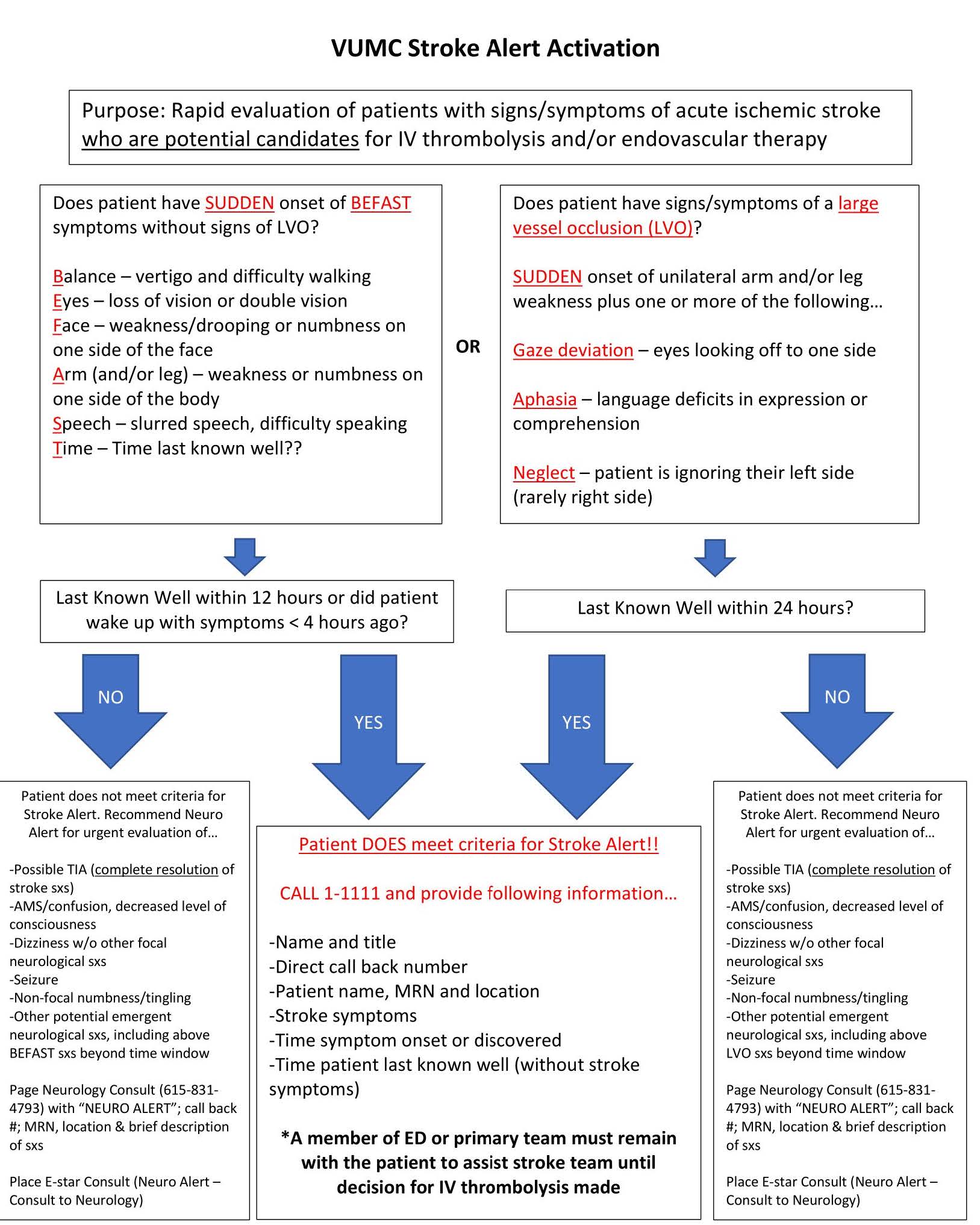
- If LKN within 24 hours and patient having persistent symptoms, then call a Stroke Alert! Purpose of Stroke Alert is to work pt up for acute treatment (thrombolytics and thrombectomy).
- VUMC: Call 11111 and tell the operator stroke alert and current pt location. It is helpful to call down to the CT techs to determine what scanner the patient will be going to and order a stat CT perfusion (CT head noncontrast and CTA head/neck also included in this order set in Epic).
- NAVA: Dial 911 from a VA landline and tell them you want to call a Stroke Alert. Use Stroke Orderset and order a CTH/CTA H/N. Consult and STAT page Neurology residents at 835-5137. Call National Tele-Stroke Provider (469-627-4790), who will run the alert with Neurology residents assisting if possible.
- STAT CT Head/CTA/CTP for consideration of TNK or endovascular therapy
- If renal function is abnormal, discuss with neurology
- MRI/MRA is an option but takes longer (MRAs are also better with Gadolinium)
- Neurology service should be leading this portion
Management
- Blood pressure goals
- Ischemic Stroke
- In general, aim is for permissive hypertension during the first 24 hours (allow SBP up to 220 if patient did not receive TNK) when in the acute phase, avoiding antihypertensives and hypotension
- Pts with high-grade stenosis, intracranial atherosclerosis may require higher BP to maintain perfusion
- Hemorrhagic Stroke
- In general, SBP goal <140, range 130-150 but no need to press if running less
- Ischemic Stroke
- Leave thisQ1H neuro checks
- Ischemic stroke
- EKG/telemetry
- TTE with Contrast to assess for intracardiac thrombus/PFO
- A1c with goal <7.0% o LDL with goal <70
- Hemorrhagic stroke
- Reverse coagulopathies
- Repeat head imaging typically 6 hours after initial scan to monitor for stability of bleed
- Typically avoid antiplatelets and anticoagulation
- Obtain MRI brain with and without contrast to evaluate for underlying etiology
***Neuro alert is no longer in effect. Can place an urgent neurology consult instead.
