Brown Recluse Bites (Loxoscelism)
Ashley Zeoli and Matthew Kern
Background
- Only a handful of spiders are truly harmful to humans
- The brown recluse (a member of the Loxosceles genus) is widespread in the South, West, and Midwest US
- They are often found in homes (attics, basements, cupboards) and outdoors (rock piles and under tree bark)
- Their numbers increase in association with humans (i.e. synanthropic)
- Appearance/identification:
- Three pairs of eyes, a monochromatic abdomen and legs, very fine hairs on legs
- Using the “violin” pattern on its body is a poor way to identify this spider, as other harmless spiders can have similar markings
- Loxoscelism is the medical manifestation of the brown recluse spider bite
- Venom contains insecticidal toxins, metalloproteases, and phospholipases
Presentation
- Bites are most common on the upper arm, thorax, or inner thigh
- Local signs:
- Usually painless, but can cause burning sensation with two small cutaneous puncture marks with surrounding erythema o Usually appears as a red plaque or papule with central pallor, sometimes with vesiculation
- Usually self-resolves in 1 week
- Skin necrosis (10-20% of cases): o Lesion can progress to necrosis overall several days
- An eschar will form that eventually ulcerates o Usually will heal over several weeks to months
- Systemic signs (rare, but more common in children):
- The degree of systemic effects does not correlate with the appearance of the bite
- Symptoms develop over several days, and include nausea, vomiting, fever, rhabdomyolysis, malaise, acute hemolytic anemia, significant swelling from head/neck bites that can compromise the airway, DIC and renal failure. Myocarditis is a rare adverse effect that may occur.
Evaluation
- Presumptive diagnosis is based clinical presentation of the bite/wound
- DDx includes vasculitis, pyoderma gangrenosum, cellulitis, or other arthropod bites
- Definitive diagnosis is based upon observing a spider bite in combination identification by an entomologist
- Patients with local symptoms do not need any further workup
- Patient with any systemic symptoms require lab evaluation for more serious disease:
- CBC, UA to eval for “blood” without RBCs, CMP, CK
- If anemia: Type and Screen, peripheral smear, reticulocyte count, LDH, haptoglobin, coags to evaluate for hemolysis or DIC
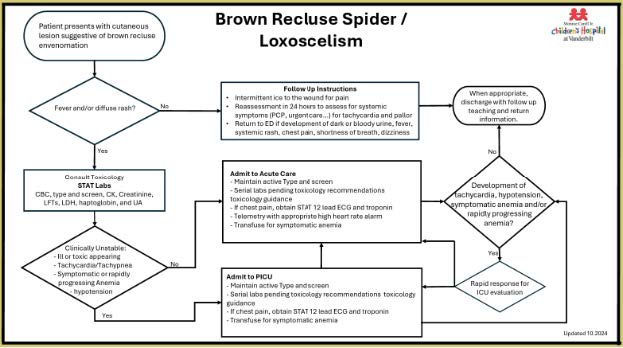
Flowchart of management protocol borrowed from VUMC Children’s Hospital.
Management
- Local signs:
- Wound care (soap/water, elevation)
- Pain management
- Tetanus vaccine/prophylaxis if indicated
- Antibiotics only if signs of concurrent cellulitis
- Skin necrosis:
- Symptomatic and supportive care
- Surgical intervention can worsen cosmetic outcomes and is rarely indicated in the acute care setting. Skin grafting is occasionally needed for a very large ulcerative wound that is not healing. Infection is rare, Furthermore, the ulcerative base of the wounds often have a yellow stringy material that is not pus or infection. Please call Toxicology with any questions regarding brown recluse bites
- Systemic signs: Targeted at treatment of symptoms that develop (Consult toxicology)
- Hemolytic anemia: generally, transfuse to keep hgb > 9-10. However, the rapidity of hemolysis is more important than the hgb for determining when to transfuse but almost always the threshold is higher than other forms of anemia.
- Rhabdomyolysis: LR for UOP >200-300cc/hr
- If patient develops chest pain: obtain EKG and check a troponin; if either is abnormal please obtain echo and call Toxicology as heart effects (i.e. myocarditis) is something we have been seeing at VUMC
- DIC: supportive care
